Dr. Langie hat einen Abschluss in Zahnmedizin an der Bundesuniversität von Rio Grande do Sul (UFRGS) (2007). Er war Praktikant in der Mund-, Kiefer- und Gesichtschirurgie (MKG) an der Zahnmedizinische Fakultät (UFRGS) (2008) und erhielt ein CAPES-Stipendium als Masterstudent in Zahnmedizin/MKG (UFRGS) (2012). Spezialist für MKG durch den Bundesrat für Zahnmedizin (CFO) (2013). Dr. Langie wurde in klinischer Forschung an der Harvard Medical School - PPCR (2013) ausgebildet. Er hat einen Doktortitel in Zahnmedizin/MKG (UFRGS), als er in Zusammenarbeit mit dem Universitätsklinikum (HCPA) arbeitete. Er war PhD Research Fellow (CAPES-12 Monate) an der Heinrich-Heine Universität Düsseldorf (HHU) und arbeitete als Fellow an der Klinik für Mund-, Kiefer- und Plastische Gesichtschirurgie / Universitätsklinikum Düsseldorf. Er war 3 Semester Student an der Medizinischen Fakultät (HHU). Dr. Langie entwickelt MKG-Forschungsthemen mit der Gruppe von Professoren der Zahnmedizinische Fakultät der UFRGS und Kollegen der Klinik für MKG am UKD. Er hat Habilitation in Krankenhauszahnheilkunde (CFO) (2017). Dr. Langie ist Kieferchirurg am Puricelli-Institut und gehört zum klinischen Personal des Krankenhauses Moinhos de Vento in Porto Alegre (HMV), der Santa Casa de Misericórdia de Porto Alegre (SCMPA) und des Krankenhauses Mãe de Deus (HMD). Er ist stellvertretender Koordinator der Ethikkommission für die pädiatrische Forschung (CEP) am Hospital da Criança Santo Antônio (HCSA/SCMPA). Dr. Langie ist auch Professor des Spezialisierungsprogramms in MKG an der SCMPA und des Graduiertenprogramms in Logopädie der Bundesuniversität für Gesundheitswissenschaften von Porto Alegre (UFCSPA). Er ist Präzeptor des Residenzprogramms in MKGder Dental School (HCPA/UFRGS). Dr. Langie koordiniert die pädiatrische MKG-Ambulanz am HSCA. Er ist auch Collaborate Professor für das Master- und PhD-Programm in Pädiatrie an der UFCSPA. Er verfügt über Kenntnisse der portugiesischen, englischen, deutschen, französischen und spanischen Sprache. Dr. Langie hat internationale Erfahrung in Forschungszentren in Brasilien und Deutschland, er ist mit verschiedenen Zentren für Kiefer- und Gesichtschirurgie in diesen Ländern verbunden.
Dr. Renan Langie
P
Dr. Renan Langie
Mund-,Kiefer- und
Gesichtschirurgie
Mund-,Kiefer- und
Gesichtschirurgie
Berufserfahrung
Behandlungsspektrum

Orthognathic Surgery
It is estimated that nearly 5% of the UK or USA population present with dentofacial deformities that are not amenable to orthodontic treatment requiring orthognathic surgery as a part of their definitive treatment.
Orthognathic surgery can be performed to correct:
- Gross jaw discrepancies (anteroposterior, vertical, or transverse discrepancies);
- Skeletofacial discrepancies associated with documented sleep apnea, airway defects, and soft tissue discrepancies;
- Skeletofacial discrepancies associated with documented temporomandibular joint pathology;
- A disproportionately grown upper or lower jaw causes dentofacial deformities.
Symptoms
Chewing becomes problematic, and may also cause pain due to straining of the jaw muscle and bone. Deformities range from micrognathia, which is when the mandible doesn't grow far forward enough (over bite), and when the mandible grows too much, causing an under bite; all of which are uncomfortable. Also, a total maxilla osteotomy is used to treat the "long face syndrome," known as the skeptical open bite, idiopathic long face, hyper divergent face, total maxillary alveolar hyperplasia, and vertical maxillary excess. Prior to surgery, surgeons should take x-rays of the patient's jaw to determine the deformity, and to make a plan of procedures.
Indications
Surgical correction of facial skeleton discrepancies is indicated when clinical orthodontic treatment alone is not capable of providing an adequate maxillomandibular relationship and, therefore, an adequate functioning of the stomatognathic system. Orthognathic surgery involves a combined pre- and postoperative orthodontic treatment, and its direct objective is functional recovery (respiratory, occlusal, masticatory, joint), with esthetic results.
Main characteristics:
• Mandibular/mental or maxillary excessive ou reduced growth;
• Gingival smile (long face);
• Overbite or deep bite (short face);
• Facial asymmetry;
• Obstructive sleep apnea syndrome (OSAS);
• Maxilla or mandible atresia.
These alterations can be congenital or developmental, and can involve the maxillary bones transversely, in the anteroposterior and vertical directions.
Procedure
Mandible osteotomies, or corrective jaw surgeries, benefit individuals who suffer from difficulty chewing, swallowing, TMJ pains, excessive wear of the teeth, open bites, overbites, underbites, or a receding chin.
The deformities listed above can be perfected by an osteotomy surgery of either the maxilla or mandible (whichever the deformity calls for), which is performed by an oral and maxillofacial surgeon who is specialized in the working with both the upper and lower jaws.
Orthognathic surgery is also available as a very successful treatment (90–100%) for obstructive sleep apnea.
Treatment goals
Orthognathic surgery is a procedure that seeks to reestablish an adequate facial pattern in patients who present changes in the proportions and relationship between the facial bones, with functional goals and an aesthetic secundary gain.
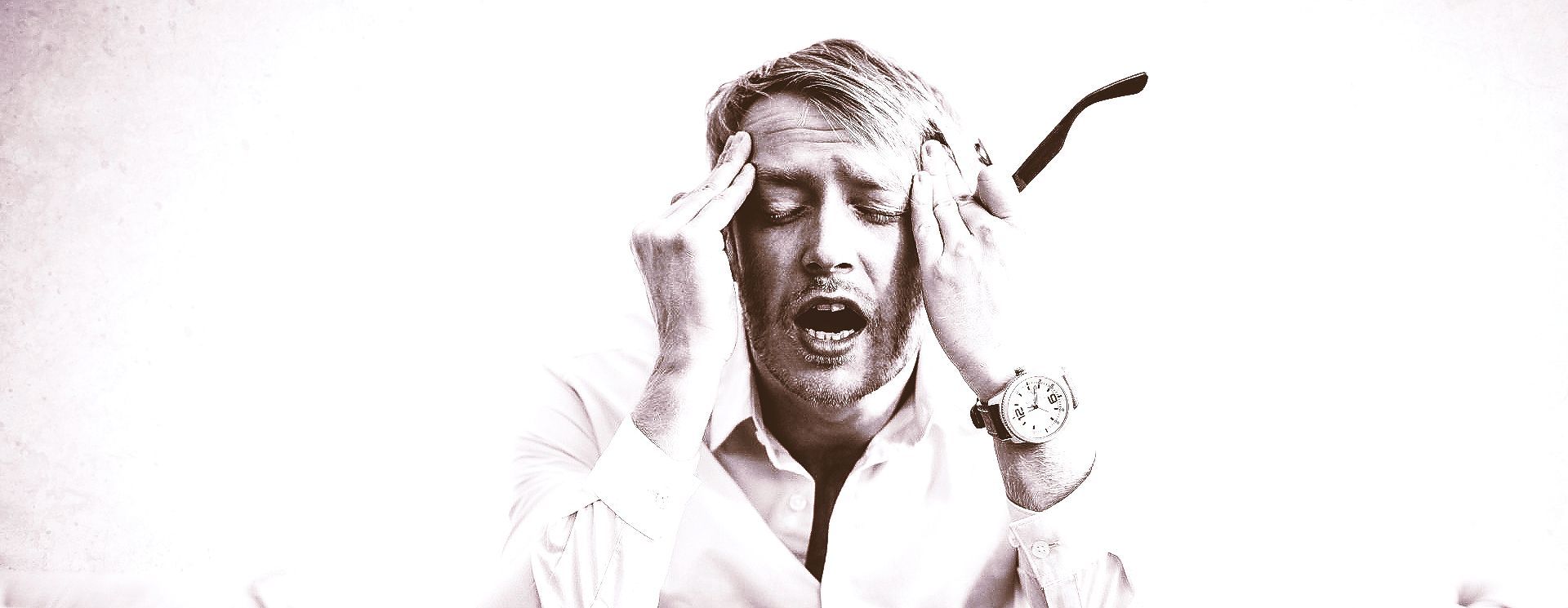
Temporomandibular Joint Disorders
The temporomandibular joint (TMJ) is the most active body joint, acting in the functions of speech, chewing, breathing, swallowing and facial expression. In general, pathologies that affect the TMJ are called Temporomandibular Joint Disorders (TMD).
TMD is a very frequent pathology, acute or chronic, and of multifactorial origin, which mainly affects women. It has an incidence of 75% in the general population, and approximately 33% of these people have at least one TMD symptom, such as headache or facial pain. Its cause is not well established, but several factors are related and contribute to the maintenance of joint dysfunction, such as parafunctional habits (such as bruxism, tooth clenching, onychophagia), changes in dental occlusion (bad dental occlusion, poorly fitted prostheses, facial skeleton), systemic diseases and emotional factors (anxiety, depression, stress).
Classification
TMDs can be divided into three types:
• Muscle disorders;
• Intra-articular disorders;
• Mixed disorders.
Symptoms
• Facial pain;
• Pain in the jaws;
• Pain in the temporal region;
• Pain in the ear;
• Pain in the TMJ region, in front of the ear;
• Pain in masticatory and accessory muscles;
• Pain during chewing;
• Headache;
• Bruxism;
• Joint noises such as clicking or crackling;
• Aural fullness (sensation of ear fullness);
• Buzz;
• Dizziness;
• Lock in mouth opening or closing;
• Restriction during mouth opening;
• Changes in dental occlusion (changes in contacts/fitting between teeth).
Diagnosis
The diagnosis of TMD is performed through physical examination and complementary exams such as Computed Tomography Scan and Magnetic Resonance of TMJs. CT scan is the ideal method for evaluating TMJ bone structures and MRI allows the study of soft tissues, including the articular disc or meniscus. On physical examination, the patient may present pain during palpation of the masticatory muscles and joint, limitation of mouth opening and mandibular excursive movements, mandible deviation during maximum mouth opening, as well as clicking and joint crackling. Changes in dental occlusion can also be observed, often associated with discrepancies in the facial skeleton or inadequate dental rehabilitation.
Treatment
Some therapeutic possibilities are:
• Occlusal splints;
• Farmacological treatment;
• Orthodontics;
• Occlusal/dental rehabilitation;
• Changing parafunctional habits;
• Physiotherapy/Speech Therapy;
• Procedures:
• Artocentesis;
• Arthroscopy;
• Viscosupplementation;
• Discopexy;
• TMJ reconstrunction.
The complexity of TMDs and their multifactorial etiology turn their treatment a challenge in the clinical practice. Therapy must be individualized, taking into account the stage of the joint disease, often requiring multidisciplinary approaches.

Snore and Obstructive Sleep Apnea
Obstructive Sleep Apnea Syndrome (OSAS) represents the complete or partial obstruction of the upper airways during sleep. These respiratory interruptions lead to a reduction of oxygen in the blood and sudden awakenings, causing sleep fragmentation and consequent release of endogenous substances that increase the risk of cardiovascular and cerebrovascular disease.
Recent studies indicate that OSAS affects about 30% of the population, and its prevalence can reach 50% of individuals in specific subgroups, including males, older individuals and those with overweight or obesity. Currently in the US, it is estimated that about 75% to 80% of patients with OSAS are not aware of their diagnosis.
Risk factors
OSAS is a multifactorial disease, and obesity is recognized as the main risk factor for the development of the condition. However, anatomical changes in the upper airway that may reduce oronasal airflow are also involved in the pathophysiology of the disease, such as nasal septum deviation, nasal concha hypertrophy, adenotonsillar hypertrophy or maxillomandibular skeletal discrepancies.
Symptoms
Snoring during sleep, whether loud or soft, is the most common symptom and usually leads the individual to seek medical help encouraged by the partner or family member. Other symptoms are also present in greater or lesser intensity depending on the severity of the disease, such as fatigue, headaches on waking up, excessive daytime sleepiness, cognitive changes, memory impairment, decreased libido, sexual impotence and mood disorders (depression/ attention deficit).
Diagnosis
Diagnosis is essential for the proper mangement of OSAS. This is perfomed through a clinical evaluation complemented by a polysomnography, which, in addition to the diagnosis, will provide information on the severity of the disease. Nasovideolaryngofibroscopy, sleep endoscopy and computed tomography of the upper airways are complementary exams that help to identify the obstruction site and can contribute to the therapeutic decision.
Treatment
Obstructive apnea treatment is performed by a multidisciplinary team and can be clinical or surgical. As it is the largest population risk factor for the development of the disease, weight loss has a positive impact on the reduction of symptoms. In addition, physical activity should be encouraged, as it helps with weight loss, in addition to increasing muscle tone. Avoiding alcoholic beverages and medications that promote muscle relaxation is also advisable. Sleep hygiene measures should be included in the daily routine.
Clinical treatment includes options for patients who do not have anatomical changes that can be surgically treated, or for those who do not have clinical conditions for surgical procedures. The intraoral appliance and positive pressure appliances (CPAP) are viable options to prevent upper airway obstruction and control OSAS.
Surgical procedures
Depending on the severity of the disease and on the site of obstruction, several surgical procedures can be performed alone or in association with the clinical treatment of OSAS, such as nasal, pharyngeal or skeletal surgery, such as orthognathic surgery, which has increasingly been considered the gold standard in the treatment of OSAS.
Skeletal surgery or maxillomandibular advancement is a surgical procedure that, through osteotomies, allows changes in the facial skeleton, aiming at widening the upper airway, consequently preventing its obstruction. It has success rates around 85%, and in approximately 40% of the cases, the disease can be cured. It is a procedure whose main advantage is the stability of long-term results.

Third Molar Removal
Indications
Surgical removal of third molars can be indicated in different situations:
• Absence of space for eruption in the dental arch;
• Risk of infection or recurrent infections (pericoronitis);
• Risk of damage to adjacent teeth (caries or resorptions);
• Inadequate positioning in the dental archleading to difficulty in cleaning and trauma to the cheek;
• Changes in the spee curve due to its extrusion;
• Orthodontic indication;
• Prevention of/or association with odontogenic cysts or tumors;
• Differential diagnosis of facial pain.
Diagnosis
The diagnosis of dental retention is performed through the association of physical dental examination with complementary exams. Among these, mainly panoramic radiography and cone beam tomography are indicated.
Procedure
The removal of impacted third molars can be performed under local anesthesia, in the dental office, or under general anesthesia, in a hospital setting. The characteristics of positioning, depth and relationship of the dental element with anatomical and vascular-nervous structures of the face, as well as the patient's general health condition, determine the anesthetic indication. Usually under local anesthesia two teeth are removed each surgical time, while under general anesthesia the 4 third molars can be removed at a unique anesthetic procedure, representing great comfort to the patient.
Post-operative care
• Cryotherapy;
• Liquid/pasty, cold diet;
• Oral hygiene as recommended;
• Sleeping with high headboard;
• Do not perform physical activities for 21 days;
• Do not expose to the sun or intense heat for 45 days;
• Use drugs as prescribed;
• Schedule return for follow-up and suture removal.
Surgical complications
• Paresthesia (temporary or permanent loss of lip/tongue sensitivity), treated with the use of multivitamins and laser therapy;
• Oroantral fistula (communication between the oral cavity and the maxillary sinus), treated at the same or a new surgical time through local flaps;
• Displacement of the dental element to natural cavities (such as the maxillary sinuses), treated at the same surgical time through maxillary antrostomy;
• Atypical jaw fractures, treated conservatively or through rigid internal fixation at the same or new anesthetic time.
Performing the removal of included third molars with a Oral and Maxillofacial Surgery specialist reduces the risk of trans- and postoperative complications.

Cists and Benign Tumors
The pathologies that affect the stomatognathic system comprise a very heterogeneous group. Some have the possibility of clinical diagnosis, while others require the association of complementary imaging and even anatomopathological exams to define a definitive diagnosis.
Most frequent pathologies
Odontogenic cysts
• Periapical inflammatory cyst;
• Keratocyst;
• Dentigerous cyst.
Benign tumors of the jaws
• Odontoma;
• Fibrous dysplasia;
• Ameloblastoma;
• Lymphangioma;
• Papilloma;
• Inflammatory hyperplasia;
• Fibroma.
Salivary Gland Pathologies
• Sialolithiasis (salivary calculus);
• Sialodenitis;
• Ranula;
• Mucocele.
The maxillofacial surgeon also works by performing biopsies of lesions with suspected malignancy (cancer of the mouth and oropharynx), together with a stomatologist, an oral and maxillofacial pathologist, and a head and neck surgeon.

Pediatric Maxillofacial Surgery
The main pathologies treated during childhood and adolescence are:
• Short labial and/or lingual frenulum;
• Natal or neonatal teeth;
• Extra-numerary teeth;
• Included teeth;
• Odontogenic cysts or tumors;
• Hamartomas;
• Syndromes with facial deformities;
• Obstructive sleep apnea;
• Changes in craniofacial growth;
• Tooth eruption delays;
• Dental malocclusions and congenital or developmental skeletal discrepancies.
The maxillofacial surgeon also follows the craniofacial growth and development of the jaws and dentition.
Depending on the patient's age, degree of understanding and cooperation, surgical technique and the existence of comorbidities, surgical procedures can also be performed under local anesthesia assisted by an anesthesiologist, sedation or general anesthesia in a hospital.

Facial Skeletal Deformities
Facial deformities include complex defects and malformations of the facial skeleton. The main conditions are associated with syndromes, such as:
• Lip, alveolar, palatal and facial;specialist in lefts;
• Goldenhar syndrome;
• Treacher Collins Syndrome;
• Crouzon Syndrome;
• Pierre-Robin Syndrome;
• Apert's Syndrome;
• Turner Syndrome.
Treatment
The treatment of facial deformities is individualized, as the clinical characteristics and degree of skeletal involvement vary. The therapy involves usually numerous reconstructive surgical phases, with grafts, osteotomies of facial bones, local and regional flap rotations, as well as osteodistraction techniques.
Multidisciplinary follow-up is essential, usually involving a geneticist, psychologist, speech therapist, plastic surgeon, orthodontist, otorhinolaryngologist, ophthalmologist, neurosurgeon and maxillofacial surgeon.

Maxillofacial Reconstruction Surgery
Reconstructive surgery of the facial skeleton is indicated in situations of loss of bone substance in the face, related to sequelae of traumatic events, resection of tumors or excision of cystic lesions. Skeletal reconstruction techniques can also be applied in the correction of facial deformities.
Main indications
• Reconstruction of facial bones and jaws through autogenous and allogeneic bone grafts;
• Mandibular reconstruction with a costal or costochondral graft;
• Mandibular reconstruction with a vascularized fibular free flap;
• Reconstruction of the orbital floor with a skullcap graft;
• Maxilla reconstruction with iliac crest graft;
• Reconstruction of edentulous ridges with autogenous grafts for the purpose of rehabilitation using dental implants;
• Sinus lift with allogeneic graft associated with autogenous iliac crest graft.
Reconstructive techniques may require a multidisciplinary approach, especially when the graft donor area is not within the maxillofacial surgeon's area of competence.

Facial Traumatology
Trauma is the third leading cause of death in Brazil. Facial trauma affects between 5% and 8% of these patients, more frequently in young people. Its effects depend on the energy, impact vector and duration of the trauma, causing mild injuries such as soft tissue and teeth injuries (from simple tooth fracture to complete avulsion), or more severe cases leading to facial bone fractures: Mandible, Maxilla , Nose, Zygoma and Orbit.
Etiology
• Urban or domestic violence;
• Traffic accidents;
• Falls;
• Sports accidents.
Symptoms
• Pain;
• Edema;
• Bruise;
• Dental mobility;
• Limitation of mouth opening or closing;
• Changes in dental occlusion (teeth fit);
• Visual alteration or double vision;
• Difficult breathing;
• Bleeding.
Diagnosis
The diagnosis of traumatic injuries follows the ATLS international guidelines, and injuries are treated with priority related to life risk. Diagnosis of facial soft and hard tissue injuries is performed through physical examination and complementary exams with radiographs and computed tomography (CT) scans with three-dimensional reconstructions.
Treatment
Soft tissue injuries may require care and sutures/dressings. Fractures of facial bones can be treated in different ways, from clinical follow-up and follow-up to surgical procedures for alignment and fixation of the bones in their anatomical position. When facial fractures are not properly treated, complications can occur, such as: infection, chronic pain, permanent double vision, change in the position of the occlusal globe, change in bite and difficulties in chewing and breathing.
Early and adequate diagnosis and treatment are essential for a good prognosis and functional and esthetic recovery.
Krankenhäuser
We offer surgical procedures at the main hospitals in town: Santa Casa de Misericórdia de Porto Alegre (SCMPA), Hospital Moinhos de Vento (HMV) and Hospital Mãe de Deus (HMD), according to your will and your health insurance contract.
Our partner teams of anesthesiologists are specially selected for your safety (SANE and SAPE).
Krankenversicherungen

*Contact your health insurance company and our secretary for further information regarding your contract and OMFS treatment coverage.
Lageplan
Hospital Ambulatory - Santa Casa de Misericórdia de Porto Alegre
Rua Professor Annes Dias, 295 - Centro Histórico, Porto Alegre
©2022 Prof. Dr. Renan Cavalheiro Langie. All rights reserved. Designed by escala.